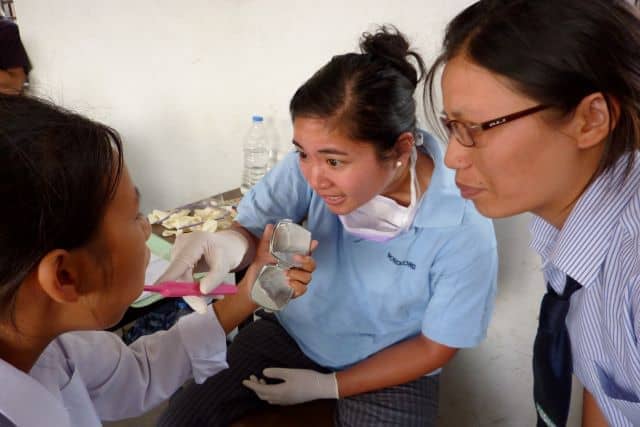
Oral Health Disparities: What CHWs Can Do
The mouth is just as important to overall health and wellbeing as any other part of the body. A simple infection can lead to a stroke and possibly death. People who work with people’s teeth understand the mouth provides an entry to the whole body. They see first-hand how the mouth can reflect problems around …