The mouth is just as important to overall health and wellbeing as any other part of the body. A simple infection can lead to a stroke and possibly death.
People who work with people’s teeth understand the mouth provides an entry to the whole body. They see first-hand how the mouth can reflect problems around the body and how problems with the mouth can affect health. Poor oral health can correlate to chronic conditions ranging from heart disease to diabetes to brain degeneration—and more.
Almost all Americans have experience with this in some way. Over 90% have at least one tooth that’s been treated for decay or needs to be. About a quarter of U.S. adults between 20 and 64 need a filling. Cavities are the most common chronic childhood infectious disease. Periodontal disease is also tragically undertreated in the States and affects about half of us. The problem there is that people with gum disease are 2 to 3 times more likely to have cardiovascular problems.
Core Competencies for CHWs
Register now for this foundational course and save with the Early Bird Discount.
COVID-19 and Dental Care
Unfortunately, since the beginning of the coronavirus pandemic, many people have been skipping oral care. According to a recent poll, 78% of respondents put off medical services, the most commonly missed being dental exams.
A person with periodontal disease is more likely to have severe results of a COVID-19 infection. That’s a troubling fact, because nearly half of all adults over 30 have periodontal disease, according to the CDC. Oral Health Disparities
Cost is another huge barrier to dental care. In the last two decades, dental care costs have risen by 30%. But many people don’t have dental insurance.
Some communities are disproportionately affected by dental and oral diseases. These are in many cases the same communities that have limited access to health services.
Access to health care and proper education helps address this gap, but there are stark disparities in the oral health of men, women, and children. These oral health disparities can have serious consequences, which we explore in depth in the CHWTraining course Oral Health Disparities.
Some of the statistics from our course are unsettling.
“Blacks, non-Hispanics, and Mexican Americans aged 35–44 years experience untreated tooth decay nearly twice as much as white, non-Hispanics,” according to the CDC. Latino children have higher rates of tooth decay, rampant decay, and treatment need, compared to non-Latino white children.
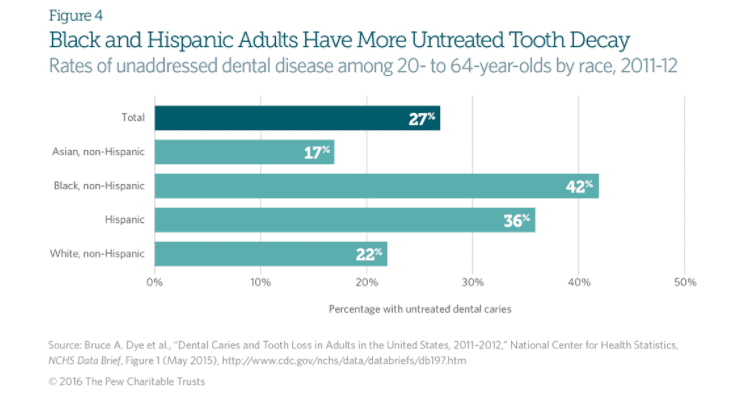
Image: Pew Charitable Trusts
Education is widely lacking. Many women aren’t aware that women have unique oral health concerns, despite regular checkups and experience with recurring canker sores and inflamed gums. Are most pregnant women told they are far more likely to have gum disease or loose teeth or that morning sickness is a problem for teeth? Probably not.
The trouble is that too few of the people in charge see it that way. Starting from the top with health policy all the way down to children who haven’t learned to brush regularly, too many people don’t know about the connection between oral and overall health.
Many people can’t afford dental insurance or expensive electronic toothbrushes or a house where the water is fluoridated, especially in underserved rural and urban areas. Still, there isn’t much care coordination and patient navigation to support people.
Fortunately, this trend is reversable because relatively simple prevention goes a long way with oral and overall health.
CHWs Can Reverse Oral Health Disparities
Communities and health systems need to step up oral health by providing better access to dentists and education. Community health workers (CHWs), promotores de salud, community dental health coordinators and other lay educators are in a perfect position to help.
States and health systems should work to include oral health education as a part of CHW training. They can help people navigate such barriers as poverty, language, geography, and even transportation. And they can do it where people live, not necessarily in a clinical setting. This is a relatively low-cost way to engage families but can have a tremendous impact a person’s health, from childhood through the rest of their life.
CHWs should also receive training in health literacy to promote better outcomes. Oral health literacy isn’t just a person’s ability to read. It’s also their ability to receive, evaluate, understand and use oral health information.
Oral health is more important than ever. Make sure your staff received the training and knowledge to pass on to clients to build their overall health. Interested in educating your team on oral health disparities? Contact us to learn how.
[mp-mc-form list=”6535a2c71c” button=”Subscribe” email_text=”Your E-mail” first_name_text=”First Name” last_name_text=”Last Name” placeholder=”true” firstname=”true” lastname=”true” success=”Thank you for joining our mailing list.” failure=”There was a problem processing your submission.” ]